Why Sprint Speed Matters in Return-to-Play
Return-to-play (RTP) decisions after injury should be guided by strong objective criteria rather than guesswork¹. Nearly one-third of hamstring strains recur within the first year of RTP², often in the first few weeks. Experts speculate that many athletes return to sport at a suboptimal performance level due to not passing RTP criteria³. In other words, if an athlete hasn’t regained the speed and power their sport demands, they’re at risk for re-injury.
One of the clearest signs of full recovery – especially in sports that involve running – is the athlete’s ability to sprint at full intensity. Sprinting is a high-demand activity, placing large forces on muscles and joints (for example, hamstring force and strain increase dramatically as running speed goes from 80% to 100% effort⁴). If an athlete can’t tolerate maximal sprinting, it suggests lingering deficits in strength, explosiveness, or confidence. Many rehab experts now include sprint speed tests as part of RTP criteria for field and court sports⁵. The goal is to ensure the athlete can handle the real-game demands: if they’ll need to chase a fast break in basketball or sprint for a ball in soccer, they must prove in testing that they can do so safely and effectively. In fact, return-to-play is often defined as returning to competition at a level comparable to pre-injury performance¹ – and sprinting ability is a key part of that for most athletes.
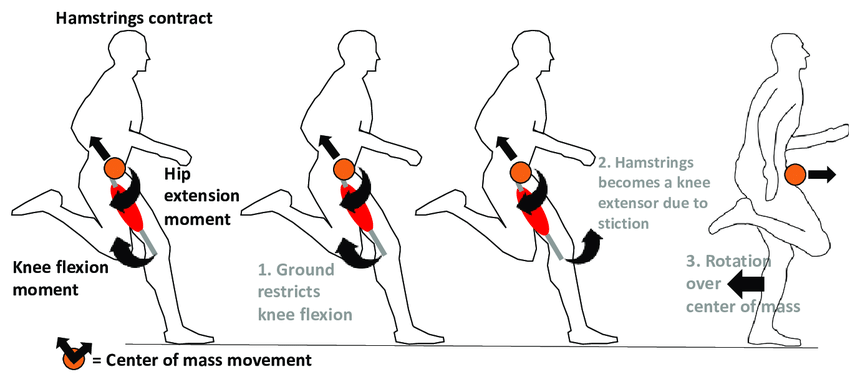
Research and professional practice back this up: multiple studies and rehab protocols list “pain-free full-speed sprinting” as a clearance criterion⁶. For example, one RTP checklist requires athletes to complete a series of progressive sprints up to 100% effort without any symptoms or hesitancy⁷. In a clinical commentary on hamstring rehab, athletes were not cleared until they could perform sprint drills at 90% of maximum speed pain-free⁸. In ACL rehab protocols for field sports, coaches often test a short sprint (like 10 m) each week and expect the athlete to reach near their pre-injury time before full return⁹. All these examples highlight the same point: sprint speed is a crucial indicator of readiness. If an athlete is still, say, 15% slower than their normal sprint time or feels pain when sprinting, it’s a red flag that more rehab or conditioning is needed before they face live competition.
When an athlete regains their sprint speed, it builds confidence for everyone involved. The athlete knows they can explode off the mark without their injury holding them back. The coach or therapist gains objective evidence that speed, power, and tissue tolerance have returned. Using sprint tests as part of a comprehensive RTP battery (along with strength tests, hop tests, agility drills, etc.) ultimately helps minimize the risk of re-injury and ensures the athlete isn’t put back into play too early⁵. In summary:
“if you can’t sprint at full speed, you’re probably not ready for full play.”
Timing Gates: A Tool for Objective Speed Testing

For measuring sprint performance, modern coaches and therapists rely on electronic timing gates. Timing gate systems are widely regarded as the tool of choice for sprint testing due to their accuracy and efficiency¹⁰. Unlike a hand-held stopwatch (which can introduce human error and reaction time delays), timing gates start and stop the clock automatically the instant the athlete passes through an infrared beam. This yields extremely precise times – often to the hundredth of a second – and removes any guesswork. Even small improvements (for example, a 0.05 second drop in a 10 m sprint) can be detected reliably with electronic timing, whereas a coach with a stopwatch might miss or mis-time such subtle changes.
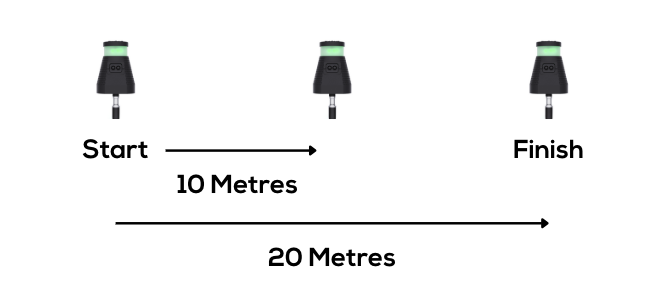
Using timing gates makes your sprint test results truly objective. The system typically includes at least two photoelectric sensors: one at the start and one at the finish of the sprint distance (additional gates can be added for split times, like 10 m and 30 m splits). When the athlete “breaks” the beam of the first gate, the clock begins; when they break the finish gate, the clock stops automatically¹¹.
Beyond accuracy, timing gates are also fast and easy to use in a training or rehab setting. Modern systems are often wireless and portable, with the ability to set up multiple gates in different configurations. Data from the gates can be logged to an app or cloud dashboard, making it simple to record results over time for monitoring progress.
Finally, timing gates provide a psychological benefit: athletes tend to give a better maximal effort when they know they’re being timed objectively. This is important for RTP testing, because a submaximal effort could give a false sense of security. With the objective feedback from timing gates, both the athlete and clinician can be confident whether the athlete has genuinely hit their top speed or is still holding back.
How To Use Timing Gates In RTP Testing

If using Timing Gates as part of Return To Play testing it is important to have a strong plan in place.
Planning the Sprint Test for Return-to-Play
Choose Relevant Distances: Select distances that match the sport’s demands. For soccer or rugby, a 10 m acceleration and a 20–30 m sprint may be ideal. Court sports often require 5–10 m sprints.
Single vs. Repeated Sprints: A single maximal sprint tests peak ability; repeated sprints add a fatigue component.
Use Baseline Data if Available: Aim for ≥90–95% of pre-injury sprint performance for clearance.
Ensure Progressive Build-Up: Only test maximal speed once the athlete has tolerated near-maximal sprinting in training.
Account for Role Differences: Tailor distances and setup to the athlete’s position-specific demands.
Best Practices for Sprint Testing with Timing Gates
Gate Setup: Place the start line ~0.3 m behind the first gate for accurate triggering¹³. Keep gate height consistent (~1 m) to avoid time variations. Use multiple gates to record split times for longer sprints.
Warm-Up: Use a consistent 10–15 min dynamic warm-up with progressive sprints.
Start Position: Standardise stance and use the same start cue each time.
Recovery: Allow 2–3 min rest between trials to avoid fatigue affecting results.
Multiple Trials: Record at least three maximal efforts and take the best time.
Consistent Environment: Test on the same surface, with the same footwear and conditions each time.
Safety: Stop immediately if pain occurs. Monitor the athlete for delayed soreness post-test.
Using Sprint Test Results to Guide Return-to-Play
- Compare to Baseline: Good = within 5% of pre-injury or normative values; Borderline = 5–10% slower; Bad = >10% slower or painful.
- Consider Symptom Response & Technique: Even if times are good, clearance requires pain-free, mechanically sound sprinting.
- Look for Consistency: Minimal drop-off across repeated sprints suggests good readiness; large declines may indicate fatigue or apprehension.
- Combine with Other Criteria: Integrate sprint data with strength, hop, and agility tests for a complete picture.
- Use Data for Confidence: Show athletes their progress to reinforce readiness or justify more training.
Integrating Timing Gate Tests into Your RTP Protocol
Introduce sprinting gradually in late-stage rehab.
Make sprint speed a formal RTP criterion alongside other objective measures.
Use split times to pinpoint acceleration vs. max velocity deficits and target them in training.
Re-test if criteria aren’t met; use data to guide final rehab.
Document results for clear communication with the athlete and coaching staff.
Conclusion
Sprinting is one of the most demanding and revealing actions in sport. By integrating timing gate sprint tests into RTP criteria, you add an objective, sport-relevant measure of readiness. This improves decision-making, boosts athlete confidence, and reduces re-injury risk. In short: if they can’t sprint at game speed in testing, they’re not ready for game speed in competition.
References
Ardern CL, Glasgow P, Schneiders A, et al. 2016 Consensus statement on return to sport from the First World Congress in Sports Physical Therapy, Bern. Br J Sports Med. 2016;50(14):853-864. doi:10.1136/bjsports-2016-096278
van der Horst N, Backx FJ, Goedhart EA, Huisstede BM. Return to play after hamstring injuries: a qualitative systematic review of definitions and criteria. Sports Med. 2016;46(6):899-912. doi:10.1007/s40279-015-0468-7
Tol JL, Hamilton B, Eirale C, Muxart P, Jacobsen P, Whiteley R. At return to play following hamstring injury the majority of professional football players have residual isokinetic deficits. Br J Sports Med. 2014;48(18):1364-1369. doi:10.1136/bjsports-2013-093016
Schache AG, Dorn TW, Wrigley TV, Brown NA, Pandy MG. Stretch and activation of the human biarticular hamstrings across a range of running speeds. Med Sci Sports Exerc. 2012;44(4):647-658. doi:10.1249/MSS.0b013e318236a3d2
Buckthorpe M, Della Villa F. Optimising the late-stage rehabilitation and return-to-sport training and testing process after ACL reconstruction. Sports Med. 2019;49(7):1043-1058. doi:10.1007/s40279-019-01102-z
Hickey J, Shield AJ, Williams MD, Opar DA. The financial cost of hamstring strain injuries in the Australian Football League. Br J Sports Med. 2017;51(22):1185-1189. doi:10.1136/bjsports-2016-096133
Silder A, Heiderscheit BC, Thelen DG, Enright T, Tuite MJ. MR observations of long-term musculotendon remodeling following a hamstring strain injury. Clin Orthop Relat Res. 2013;471(9):2933-2941. doi:10.1007/s11999-013-2945-9
Malliaropoulos N, Isinkaye T, Tsitas K, Maffulli N. Reinjury after acute posterior thigh muscle injuries in elite track and field athletes. Am J Sports Med. 2011;39(2):304-310. doi:10.1177/0363546510382856
DePaul University. ACL Rehabilitation Protocol. Chicago, IL: DePaul University Athletics; 2021.
Haugen T, Buchheit M. Sprint running performance monitoring: methodological and practical considerations. Int J Sports Physiol Perform. 2016;11(6):788-794. doi:10.1123/ijspp.2015-0330
Yeadon MR, Kato T, Kerwin DG. Measuring running speed using photocells. J Sports Sci. 1999;17(3):249-257. doi:10.1080/026404199366172
Brown SR, Brughelli M, Hume PA. Knee mechanics during planned and unplanned sidestepping: a systematic review and meta-analysis. BMJ Open Sport Exerc Med. 2022;8(1):e001314. doi:10.1136/bmjsem-2021-001314
Cronin JB, Templeton R. Timing light height affects sprint times. J Strength Cond Res. 2008;22(1):318-320. doi:10.1519/JSC.0b013e31815f2fd4

