Falls pose a significant health risk, particularly in older and clinical populations. Traditional clinical balance tests often fall short in sensitivity when predicting fall risk. Force plate posturography, however, offers objective and quantifiable measures of postural sway through center-of-pressure (CoP) movement, which can detect subtle balance impairments. Recent research highlights that CoP metrics, such as total sway excursion (path length) and sway area, correlate with fall risk and effectively distinguish high-risk individuals. This white paper summarizes recent evidence, including systematic reviews, meta-analyses, and key studies in older adults and individuals with neurological or musculoskeletal conditions.
Evidence in Older Adults (General Population)

Systematic Reviews & Meta-Analyses
Recent systematic reviews strongly support the use of force plates for fall risk screening in seniors. A 2020 review and meta-analysis, encompassing 44 studies and over 7,000 older adults, identified several CoP parameters as effective fall-risk biomarkers. Notably, sway area per unit time and CoP velocity, particularly anteroposterior and radial mean velocity, were among the most effective at discriminating fallers from non-fallers. Quiet-stance force plate tests identified individuals at high fall risk, suggesting these measures could enhance routine fall-risk assessments in clinical practice.
Additional narrative reviews indicate that older adult fallers generally exhibit larger sway (greater CoP displacement), emphasizing the value of CoP metrics in assessing balance deficits.
Sway Total Excursion
Total CoP excursion, or sway length, has been linked to fall risk. For instance, Johansson et al. (2020) found that older adults with a sway path of ≥400 mm had a 75% higher fall risk. Prosperini et al.’s meta-analysis further supported this, showing an 8% increase in fall risk for each additional 10 mm of sway path. These findings underscore that greater sway excursion during quiet standing is a precursor to fall susceptibility.
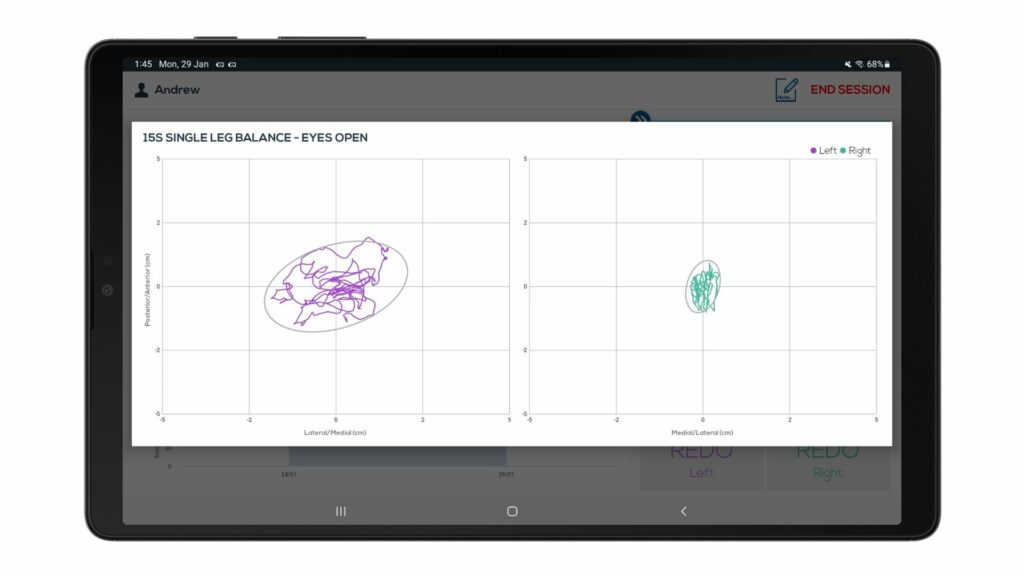
Sway Confidence Area
An enlarged sway area, such as the area of the 95% confidence ellipse of CoP, is another key risk indicator. In a study of 170 older adults, fallers demonstrated significantly poorer one-legged stance balance, including a larger CoP area compared to non-fallers. A CoP area cutoff of ~10.3 cm² (one-leg stance, eyes open) was identified as optimal for distinguishing fallers from non-fallers, with 78% sensitivity and 68% specificity. This suggests that exceeding a certain sway area threshold indicates abnormal postural sway and higher fall risk.
Prospective Studies
CoP metrics hold predictive value for future falls. In a prospective study by Bauer et al. (2016), force plate variables were significantly associated with future falls. Older adults who later experienced falls displayed greater lateral sway, particularly a higher mediolateral-to-anteroposterior sway ratio and more rapid lateral oscillations during baseline posturography. These findings suggest that force plate tests can identify subtle instabilities that precede real-life falls, often outperforming a prior fall history in predicting new falls.
Populations with Neurological Conditions
Parkinson’s Disease
Individuals with Parkinson’s Disease (PD) often exhibit characteristic sway abnormalities linked to falls. A 2023 study by Kwon et al. demonstrated that PD fallers had significantly greater CoP excursion distances, larger sway areas, and faster sway velocities than non-fallers. The increased sway, particularly in the mediolateral direction, indicates less efficient postural control in fallers. These findings support the use of force plate tests in PD fall risk evaluations to detect balance impairments, especially lateral instability, which may not be clinically apparent.
Stroke Survivors
Post-stroke survivors often experience balance deficits that can be quantified through CoP measures. Mansfield et al. (2015) found that stroke survivors with higher mediolateral sway were more likely to fall. An increased RMS amplitude of ML CoP motion related to a higher fall risk post-stroke, highlighting how force plates can identify specific postural control weaknesses that inform fall prevention strategies.
Multiple Sclerosis
Multiple sclerosis (MS) often impairs balance, with force plate assessments proving clinically insightful. Prosperini et al. (2013) showed that static posturography could predict future falls in MS patients, with sway path length emerging as a strong predictor. Subsequent studies have confirmed that force plate measures are sensitive, detecting subtle CoP abnormalities in minimally impaired MS patients well before clinical tests indicate issues. This enables early identification of fall risk in MS, supporting the use of force plates for balance assessment and fall prevention.
Populations with Musculoskeletal Conditions
Musculoskeletal disorders, such as osteoporosis and arthritis, as well as general frailty, contribute to falls. CoP-based posturography is a valuable assessment tool in these cases. Moon et al. (2024) identified significant differences in sway metrics between osteoporotic individuals who had recently fallen and those who had not. Fallers exhibited higher sway path lengths, larger sway areas, and faster CoP shifts, aligning with poorer musculoskeletal health markers. Similar trends are seen in conditions like knee osteoarthritis, where balance training and force plate–based biofeedback exercises have shown significant improvement in CoP sway metrics, indicating better balance and fewer stumbles.

Practical Applications and Considerations
Force plate CoP testing offers significant clinical applications for fall prevention. Research suggests incorporating brief force plate balance tests into geriatric assessments to improve fall-risk screening sensitivity. Quiet-standing CoP metrics provide continuous, quantitative data on postural stability, detecting risk factors not visible through standard scales. These non-invasive tests can be completed quickly and affordably, with portable force plates enabling use in small clinics and community centers.
Force plate assessments also prove valuable for tracking changes over time. Clinicians can monitor sway metrics to gauge balance improvements, stability, or deterioration in elderly or neurologically impaired patients. This is particularly useful in conditions like Parkinson’s disease, where serial posturography can track disease progression or treatment impact on balance. The objective, numeric outcomes of CoP assessments allow for quantification of subtle improvements, encouraging their use in research and therapeutic settings to evaluate intervention efficacy.
References
- Quijoux F, Vienne-Jumeau A, Bertin-Hugault F, et al. Center of pressure displacement characteristics differentiate fall risk in older people: A systematic review with meta-analysis. Ageing Res Rev. 2020;62:101117. doi:10.1016/j.arr.2020.101117
- Howcroft J, Lemaire ED, Kofman J, McIlroy WE. Elderly fall risk prediction using static posturography. PLoS One. 2017;12(2):e0172398. Published 2017 Feb 21. doi:10.1371/journal.pone.0172398
- Wiśniowska-Szurlej A, Ćwirlej-Sozańska A, Wilmowska-Pietruszyńska A, Sozański B. The Use of Static Posturography Cut-Off Scores to Identify the Risk of Falling in Older Adults. Int J Environ Res Public Health. 2022;19(11):6480. Published 2022 May 26. doi:10.3390/ijerph19116480
- Bauer CM, Gröger I, Rupprecht R, Marcar VL, Gaßmann KG. Prediction of future falls in a community dwelling older adult population using instrumented balance and gait analysis. Z Gerontol Geriatr. 2016;49(3):232-236. doi:10.1007/s00391-015-0885-0
- Oliveira MR, Vieira ER, Gil AWO, Fernandes KBP, Teixeira DC, Amorim CF, et al. (2018) One-legged stance sway of older adults with and without falls. PLoS ONE 13(9): e0203887. https://doi.org/10.1371/journal.pone.0203887
- Kwon DY, Kwon Y, Choi JA, Ko J, Kim JW. Quantitative Analysis of Postural Balance in Faller and Nonfaller Patients with Parkinson’s Disease. Parkinsons Dis. 2023;2023:9688025. Published 2023 Jun 20. doi:10.1155/2023/9688025
- Kamieniarz A, Michalska J, Brachman A, Pawłowski M, Słomka KJ, Juras G. A posturographic procedure assessing balance disorders in Parkinson’s disease: a systematic review. Clin Interv Aging. 2018;13:2301-2316. Published 2018 Nov 12. doi:10.2147/CIA.S180894
- Wiśniowska-Szurlej A, Ćwirlej-Sozańska A, Wilmowska-Pietruszyńska A, Sozański B. The Use of Static Posturography Cut-Off Scores to Identify the Risk of Falling in Older Adults. Int J Environ Res Public Health. 2022;19(11):6480. Published 2022 May 26. doi:10.3390/ijerph19116480
- Moon SH, Doshi KB, Lockhart T. Assessing fall risk in osteoporosis patients: a comparative study of age-matched fallers and nonfallers. Front Digit Health. 2024;6:1387193. Published 2024 Jul 10. doi:10.3389/fdgth.2024.1387193
- Sadura-Sieklucka T, Czerwosz LT, Kądalska E, Kożuchowski M, Księżopolska-Orłowska K, Targowski T. Is Balance Training Using Biofeedback Effective in the Prophylaxis of Falls in Women over the Age of 65?. Brain Sci. 2023;13(4):629. Published 2023 Apr 6. doi:10.3390/brainsci13040629

